One of the key priorities in modern healthcare is the continuity of care, which is impossible to achieve without robust healthcare interoperability. Essentially, interoperability refers to the ability of different systems to communicate and exchange electronic data in a safe and efficient manner.
In healthcare, the journey to interoperability began in 2009 when the HITECH Act was adopted to promote the meaningful use of electronic health records (EHR). Today, interoperability goes beyond EHRs to every healthcare system. According to MarketsandMarkets research, the global market for interoperability solutions in healthcare is estimated to amass USD 4.2 bln by 2024 growing at a CAGR of 12.6%.
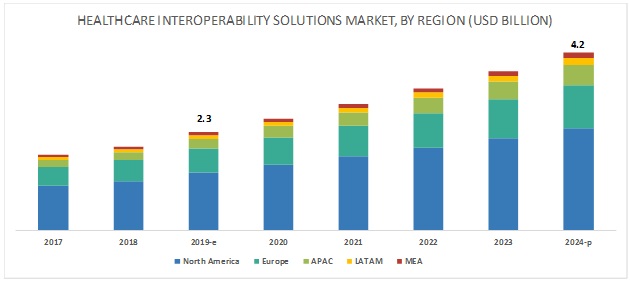 Source: MarketsAndMarkets
Source: MarketsAndMarkets
What is interoperability in healthcare
According to the definition provided by the
Healthcare Information and Management Systems Society (HIMSS), interoperability is “the extent to which systems and devices can exchange data, and interpret that shared data”. Interoperability of information systems in healthcare is important for many reasons — from better patient care and improved clinical workflows efficiency to reduced errors and decreased administrative costs.
The proposed definition of interoperability in healthcare comes with four layers:
- Foundational level is the most basic tier that provides the interconnectivity requirements necessary for a system to be able to send data to another system and receive data from it.
- Structural level defines the syntax, format and structure of data exchange to ensure that information can further be interpreted.
- Semantic level refers to the ability of systems to exchange and then actively use structured messages that contain standardized data.
- Organization level encompasses governance, social, legal components in order to promote secure and seamless transmission and use of data within as well as between different organizations.
Healthcare interoperability, however, is not a straightforward process as it has a number of challenges. A survey carried out by Deloitte identifies the top three barriers to achieving interoperability, which we will further discuss in greater detail.
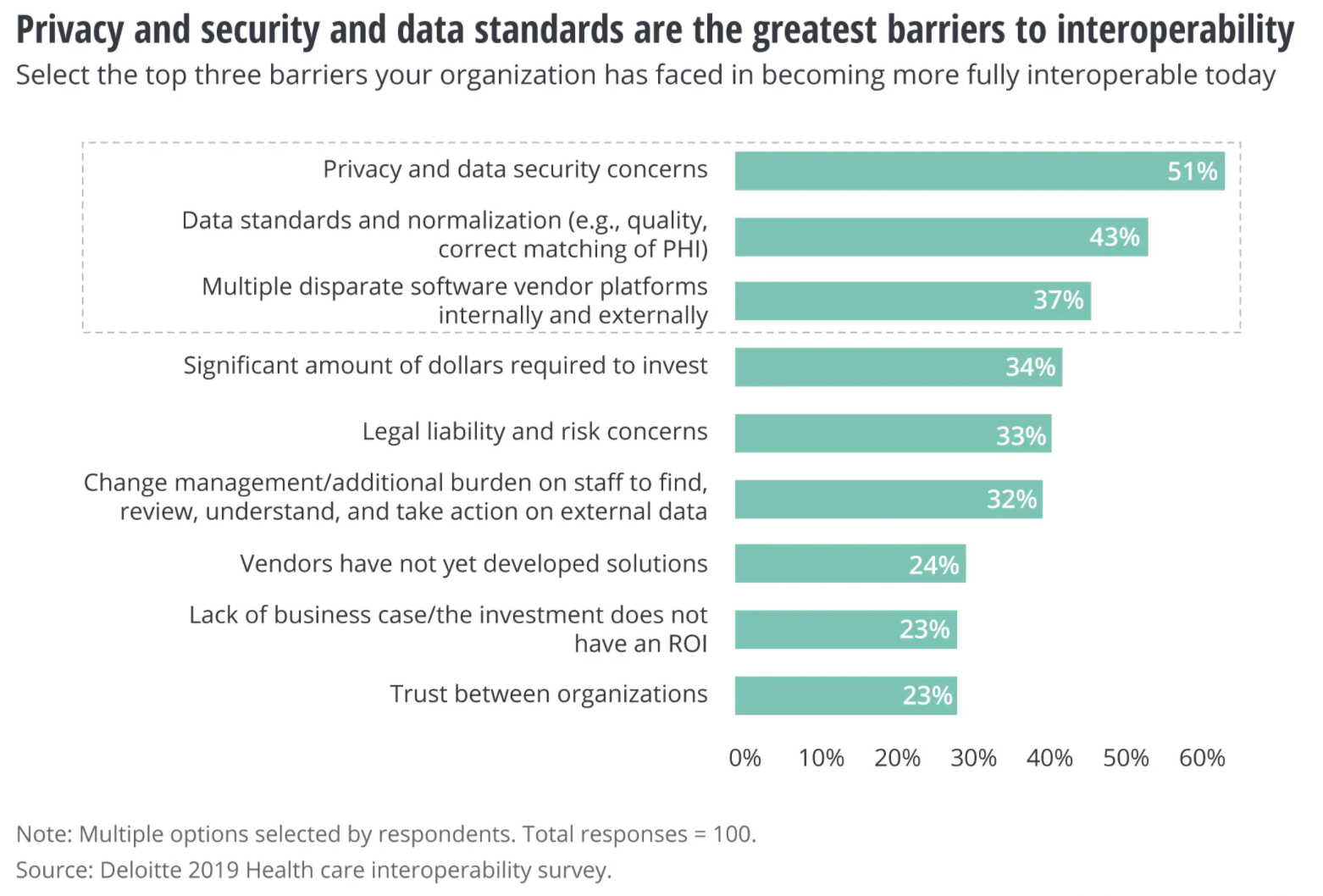
Source:
Deloitte 2019 Healthcare interoperability survey
Challenge #1. Privacy and security concerns
The majority of healthcare leadership see privacy and security issues as the top barrier to embracing health interoperability, and rightfully so. Every time a system opens to an external network, there is a risk of potential threats or even attacks. Given the sensitive nature of protected health information (PHI) exchanged between health systems, maintaining patients’ privacy and security becomes a priority for all participants of a healthcare ecosystem.
According to a report by the
Trusted Network Accreditation Program (TNAP) collaborative, 62% of respondents agreed that inconsistent privacy and security policies were hampering provider support for large-scale data exchange. Furthermore, 84% considered that privacy and security certification and accreditation could help build trust.
Addressing the challenge:
- HIPAA compliance. Health information systems must comply with the Health Insurance Portability and Accountability Act (HIPAA) that prescribes the necessary safeguards to guarantee the privacy of sensitive patient information.
- Security by design and by default. To ensure robust patient data protection, security considerations must be implemented already at the design phase including, patient authentication, secure connection protocols, data minimization, and more.
- Comprehensive security testing. End-to-end security testing of APIs, connectors, and interfaces can help identify and mitigate any security vulnerability.
Challenge #2. Inconsistent patient identification standards
To ensure accurate data sharing and consistent patient matching across the entire care continuum, a unique patient identifier is a must. HIPAA creators realized that back in 1996, but the initiative was severely criticized for privacy reasons and consequently banned by Congress two years later.
However, the need for a national patient identifier (NPI) remains strong since patient identity mix-ups and errors continue to grow exponentially as healthcare providers now exchange health information on a much larger scale. Mismatches in patient identification not only lead to duplicate records and increased administrative costs but also cause a higher risk of incorrect diagnosis and mistreatment.
Healthtech startups are actively participating in the collaborative push to improve patient matching and drive interoperability. The Workgroup for Electronic Data Interchange (WEDI) and the National Association for Trusted Exchange (NATE) work on the
Virtual Clipboard Initiative that aims to automate the collection of demographic and insurance data in order to simplify the exchange and coordination of patient data.
Addressing the challenge:
- Several data elements for more accurate matches. Healthcare providers can use the combination of first and second names, sex, date of birth, social security number, and other components for more quality matches.
- Biometrics-based identification. Fingerprints, voice and face recognition, and even iris scans can serve as a unique patient identifier and help associate the right information with the right patient.
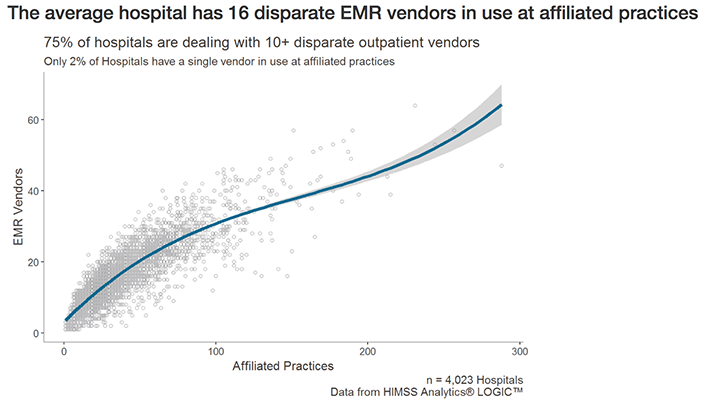
Another part of the problem is the sheer amount of EHR and EMR software providers and, more specifically, the number of platforms an average hospital is running. HIMSS Analytics looked at over 570 thousand providers affiliated with 4,023 hospitals and discovered that an average hospital uses 16 different EMR vendors.
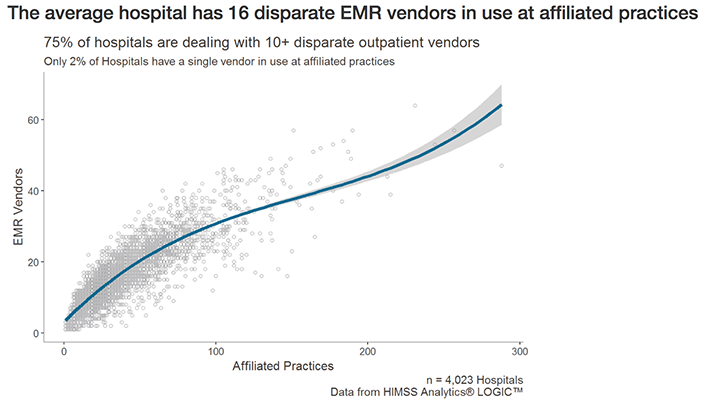
Source:
Healthcare IT News
In reality, EHRs and EMRs are just one piece of the puzzle. Today, hospitals and medical practices rely on complex ecosystems of solutions and applications — billing systems, patient management software, administrative systems, and more — to automate and facilitate complex clinical workflows. Delivered by different vendors, these systems often come with proprietary communication protocols, making healthcare providers spend scarce resources setting each solution in a unique, interoperable way.
Addressing the challenge:
- Compliance with the applicable interoperability standards in healthcare. The most widely recognized standard is FHIR (Fast Healthcare Interoperability Resources), but depending on the data type and processes, your healthcare solution may need to comply with DICOM for sharing medical images, ICD-10 for standardizing diagnosis codes, HL7 V3 for transferring demographic and administrative data, and other standards.s
- Leveraging the power of the cloud. Implementing cloud-native healthcare solutions can also improve interoperability by breaking down data silos while improving patient data safety.
The barriers are surmountable
The importance of healthcare interoperability can hardly be overestimated. Transitioning to value-based care, streamlining patient experiences, and reducing healthcare costs require seamless data exchange between all the participants of the healthcare continuum, from patients to healthcare providers and pharma and insurance organizations.
And although there is still a long way to go towards full healthcare interoperability, industry leaders and healthtech companies can now prioritize interoperability initiatives and focus on overcoming top barriers through adopting cloud computing, protecting privacy and confidentiality of patient data and supporting regulatory compliance, among other things.

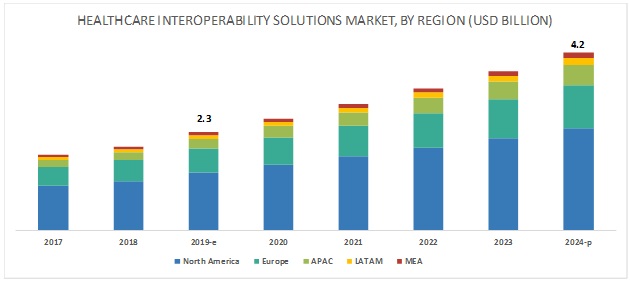 Source: MarketsAndMarkets
Source: MarketsAndMarkets
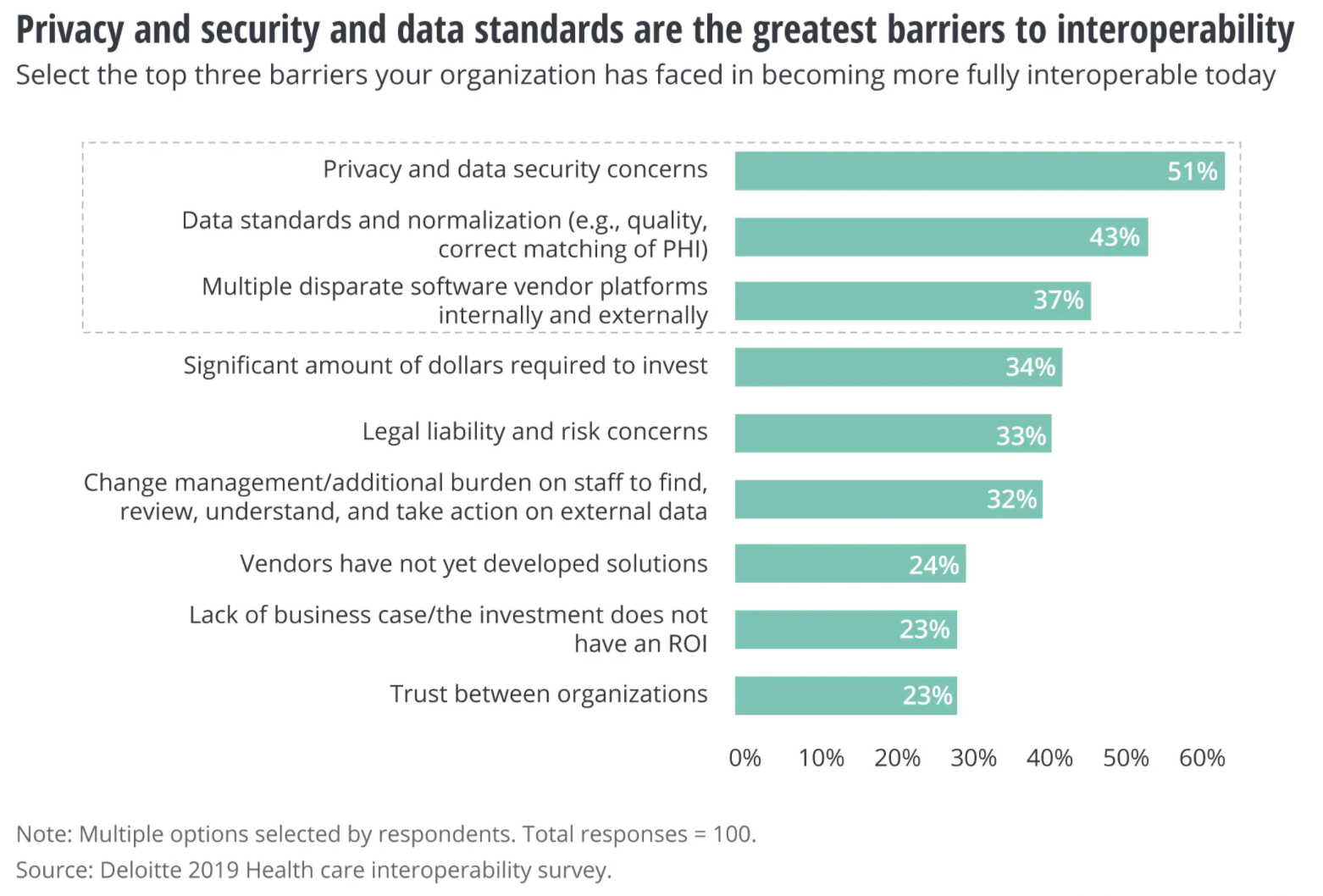 Source: Deloitte 2019 Healthcare interoperability survey
Source: Deloitte 2019 Healthcare interoperability survey