May 22, 2025
Healthcare
Enhancing Oncology Care with Digital Interventions for Treatment and Monitoring
Cancer care is one of the most complicated challenges in medicine–diagnosis is nuanced, treatment is highly personalized, and the patient journey is long and emotionally loaded, all while being expensive. In the U.S., cancer accounts for about 7% of total healthcare spending.
But digital health is finally starting to change how we manage this complexity. Whether it’s remote monitoring, better diagnostics, or AI-supported decisions, these tools are giving clinicians and patients ways to catch issues earlier, respond faster, and stay out of the hospital longer.
A real-world example showed that across 33 cancer centers in Europe, rolling out a digital symptom monitoring program helped nearly 95% of patients improve within two weeks after an alert. That’s not hypothetical. That’s just better care.
 Patient-reported symptom grades (PRO CTCAE) before and after digital alert interventions.
Source: The Lancet
Patient-reported symptom grades (PRO CTCAE) before and after digital alert interventions.
Source: The Lancet
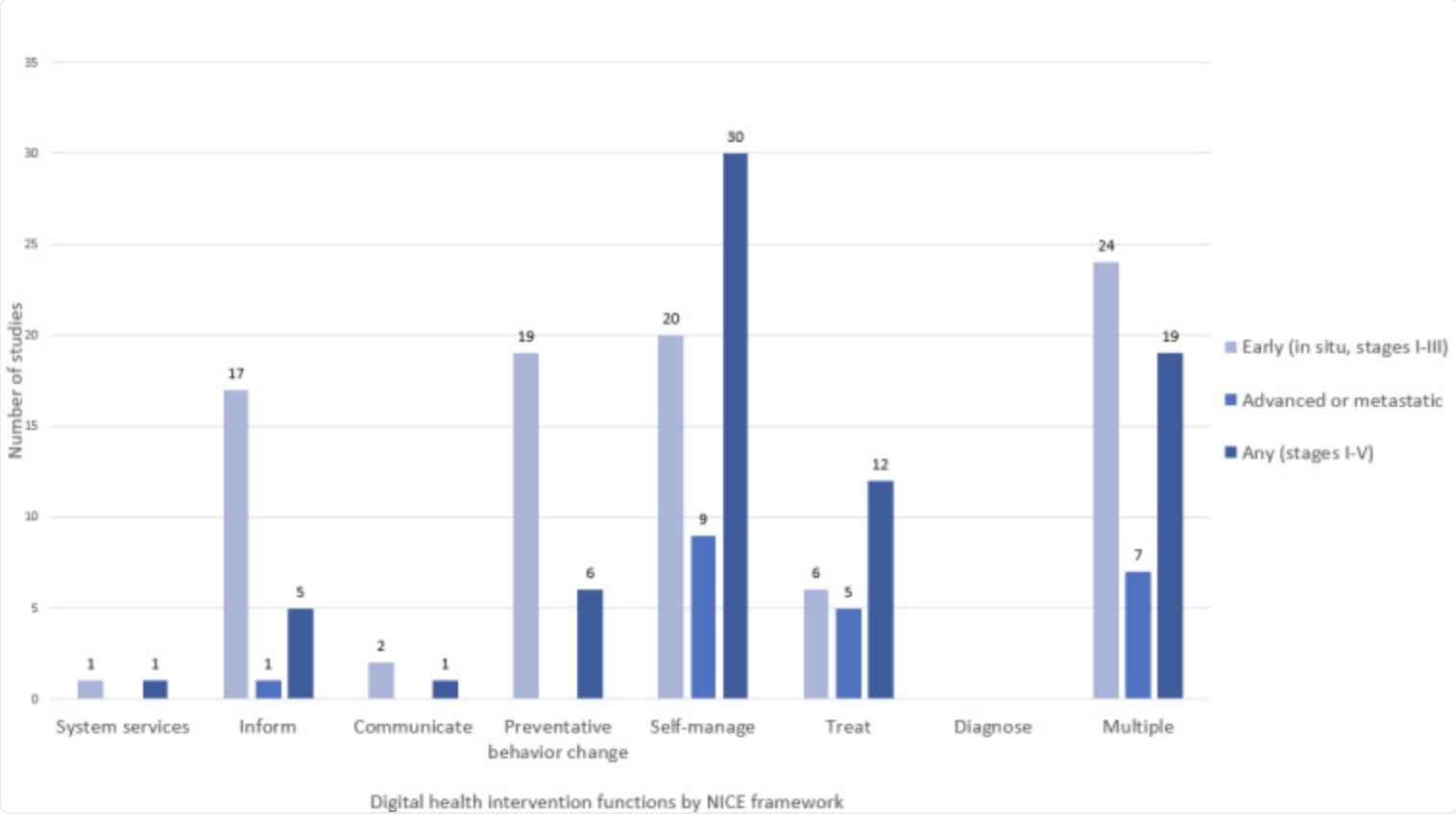 Digital health intervention functions by cancer care phase. Based on NICE framework categories.
Source: PubMed Central
Some of the biggest shifts are happening in four areas: remote monitoring, telemedicine, advanced diagnostics, and data-powered clinical support. Oncology may have lagged behind other fields in going digital, but the upside here is enormous, especially given how fast costs and complexity are rising.
Digital health intervention functions by cancer care phase. Based on NICE framework categories.
Source: PubMed Central
Some of the biggest shifts are happening in four areas: remote monitoring, telemedicine, advanced diagnostics, and data-powered clinical support. Oncology may have lagged behind other fields in going digital, but the upside here is enormous, especially given how fast costs and complexity are rising.
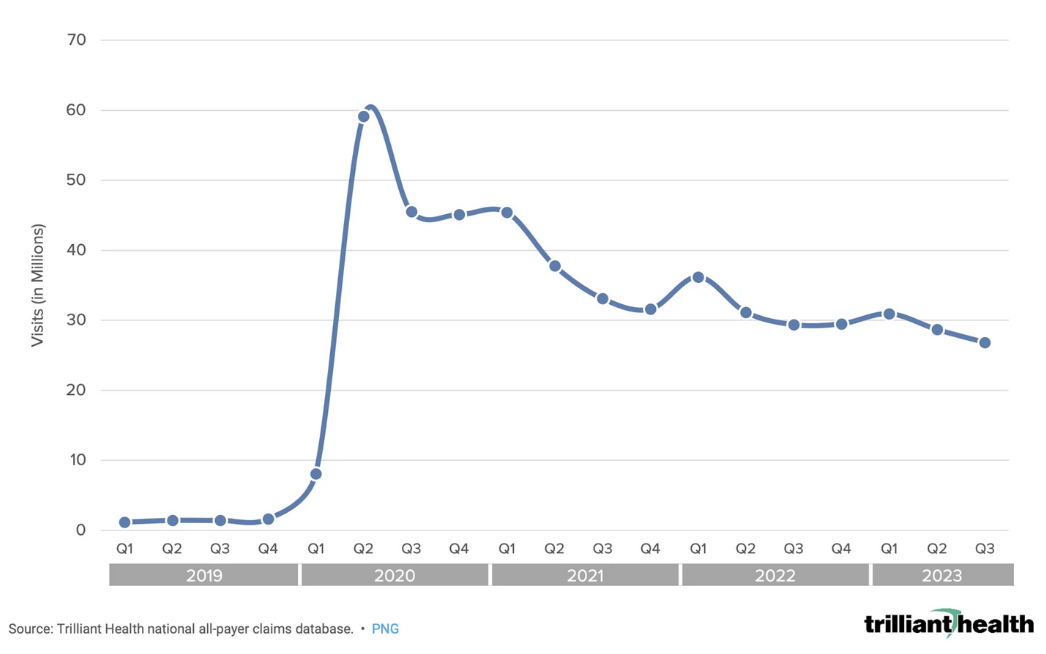 Quarterly telehealth visit volume Q1 2019 – Q3 2023.
Source: Trilliant Health
Quarterly telehealth visit volume Q1 2019 – Q3 2023.
Source: Trilliant Health
 Patient-reported symptom grades (PRO CTCAE) before and after digital alert interventions.
Source: The Lancet
Patient-reported symptom grades (PRO CTCAE) before and after digital alert interventions.
Source: The Lancet
How are digital interventions transforming oncology care?
Digital health in oncology is a growing network of systems designed to collect data, connect people, and support decisions. This transformation spans the entire journey: screening, diagnosis, treatment, recovery, even survivorship.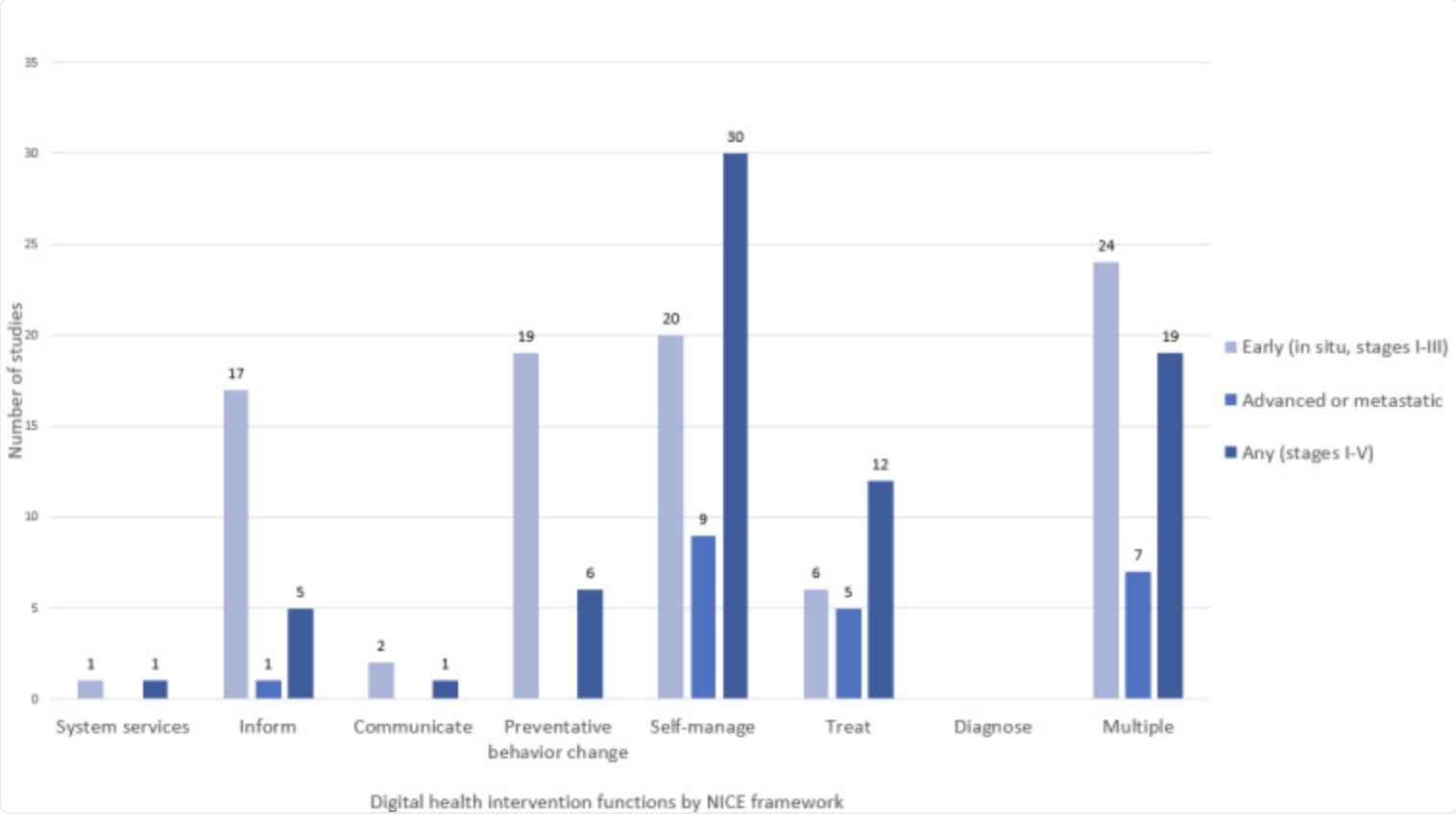 Digital health intervention functions by cancer care phase. Based on NICE framework categories.
Source: PubMed Central
Some of the biggest shifts are happening in four areas: remote monitoring, telemedicine, advanced diagnostics, and data-powered clinical support. Oncology may have lagged behind other fields in going digital, but the upside here is enormous, especially given how fast costs and complexity are rising.
Digital health intervention functions by cancer care phase. Based on NICE framework categories.
Source: PubMed Central
Some of the biggest shifts are happening in four areas: remote monitoring, telemedicine, advanced diagnostics, and data-powered clinical support. Oncology may have lagged behind other fields in going digital, but the upside here is enormous, especially given how fast costs and complexity are rising.
Can remote patient monitoring improve cancer treatment journeys?
Remote patient monitoring (RPM) uses wearables and mobile tools to track patients outside the clinic. The tech may be simple, like a smartwatch or a phone app, but the benefits are real.Continuous health tracking
Devices track heart rate, oxygen levels, activity, sleep, and more. Some tools even collect patient-reported symptoms through passive prompts, like daily check-ins. A growing body of research is focused on how wearable tech fits into cancer care, and it’s looking promising.Early detection of side effects
Continuous monitoring allows for the early identification of treatment side effects or complications. For instance, a patient experiencing nausea or decreased oral intake might report this via a text-based PRO system, triggering timely intervention like IV fluid administration, potentially avoiding emergency visits, as illustrated by the comparative patient experiences described in the JNCI article. Passive activity monitoring has even been associated with reduced hospitalizations and improved survival in some trials.More control, less disruption
Fewer in-person visits means less travel, lower infection risk, and fewer disruptions for patients already juggling a lot. For many, it’s simply a better way to live with cancer.What role does telemedicine play in oncology patient support?
Video visits and remote consults have become a fixture since COVID, but in oncology, they’ve proven especially valuable.Closing the distance gap
For rural patients or those far from major cancer centers, telemedicine opens up access to top-tier specialists. A study in PMC shows that real-time video consults between oncologists and patients hundreds of miles apart can match the quality of in-person care.Faster coordination
These platforms support not just patient-doctor visits, but also doctor-to-doctor consults. That means quicker decisions, more accurate plans, and fewer silos.Mainstream adoption
In the early days of the pandemic, some cancer centers saw 70% of visits shift to telehealth. What started as a stopgap is now a core part of care.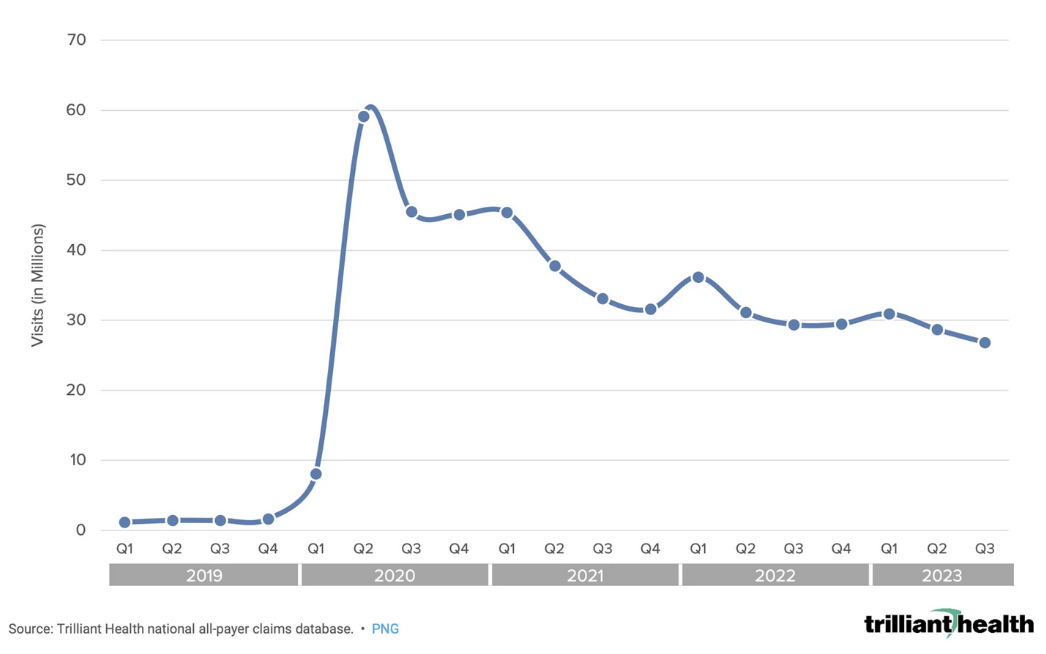 Quarterly telehealth visit volume Q1 2019 – Q3 2023.
Source: Trilliant Health
Quarterly telehealth visit volume Q1 2019 – Q3 2023.
Source: Trilliant Health
How do digital tools support earlier cancer detection and diagnosis?
It’s not just about managing known conditions, digital tools are enhancing early detection and diagnostic capabilities.- Digital screening and self-assessment: Apps now guide users through symptom tracking and self-checks, sometimes backed by AI to flag warning signs. The goal is to reduce late-stage diagnoses.
- More precise diagnostics: From genomic testing to liquid biopsies, digital tools help parse tumor genetics and detect biomarkers in blood, with no invasive procedures required. On top of that, AI is being used in radiology and pathology to scan images faster and more accurately than human eyes alone.
Turning Data Into Better Treatment Plans
All this progress depends on one thing: better data, and knowing how to use it.Smarter use of EHRs
Electronic health records centralize vast amounts of patient data. When structured properly, EHR data can power clinical decisions, track outcomes, and drive research. Natural language processing (NLP) tools are even starting to mine doctors’ notes for insights. Kanda explores NLP in medical software for diagnostic assistance here.Predictive models
Machine learning algorithms are now analyzing everything from vitals and genomics to patient-reported symptoms. They’re being used to flag risks, like which patients are likely to need acute care, and to tailor treatments based on predicted response.Interoperability is Key
A major barrier is still interoperability. Many platforms don’t talk to each other. Standards like FHIR (Fast Healthcare Interoperability Resources) and data models like mCODE (Minimal Common Oncology Data Elements) are helping to fix that, creating a “digital highway” for cancer data that can flow securely between systems. You can read more about virtual care transformation trends here.What are the challenges?
Digital health has momentum in oncology, but adoption isn’t without friction. There are still some major hurdles:- Data security and privacy: Cancer data is sensitive. Platforms need airtight security, and patients need confidence it’ll be protected.
- Data fragmentation: When digital tools operate in silos, the value drops fast. Interoperability is still a major bottleneck.
- Access and equity gaps: Not every patient has broadband, devices, or the digital literacy to navigate complex platforms. Tech should close gaps, not widen them.
- Reimbursement remains unclear: Some tools, like those for symptom tracking or wearables, don’t always have a clear path to reimbursement, which can stall rollout.
- Clinical workflows: Any tool that slows clinicians down, even a little, risks being sidelined. Seamless integration is non-negotiable.
Case Study Spotlight: Enabling Precision Oncology with Trapelo & Kanda
One example of what this can look like in practice is the Trapelo (now Neogenomics) platform. Trapelo gives oncologists a real-time system for precision medicine decisions. Trapelo delivers a next-generation precision medicine platform that empowers oncologists, labs, and payers (insurers) to make real-time, evidence-based decisions aligned with the latest clinical guidelines—streamlining molecular testing, reducing treatment delays, and improving outcomes for cancer patients. As demand grew, they needed better scalability, lower infrastructure cost, and top-tier security. Kanda helped them migrate to AWS, meeting HIPAA standards while improving performance. Now, the platform connects directly to EMRs, lets clinicians place and track orders in a single workflow, and provides up-to-date, evidence-based treatment suggestions. The platform helps doctors move faster, and patients get more personalized care.How Kanda Can Help
Going from idea to impact in oncology takes more than a development team. You need healthcare expertise, regulatory know-how, and the ability to scale without shortcuts. That’s what Kanda brings. We help teams build the tools that make digital oncology work.- Custom platforms: For virtual care, RPM, clinical support, and more
- AI + ML integration: From risk prediction to diagnostic augmentation
- Cloud infrastructure: Secure, HIPAA-compliant, built to scale
- Data engineering: Systems that talk to each other
Conclusion
From continuous monitoring and remote consults to more accurate diagnostics and AI-powered treatment plans, digital tools are shifting the entire model toward something more responsive, more efficient, and more patient-friendly. The challenges are real. But so is the momentum. And the organizations that figure it out are going to lead the way in delivering faster, smarter, and more patient-centered care.Related Articles

7 Ways RAG in AI Models Supports Modern Healthcare
If you’ve read our blog, then the challenges in healthcare IT are familiar ones. Data sits trapped in silos, clinicians lack quick information retrieval when it matters most, and AI tools might produce made-up answers without any warning. Large language models promised to change this, but hallucination remains a serious liability. Mayo Clinic demonstrated the…Learn More
Healthcare Web Development: The Fastest Route to Scalable Patient Care
Outdated medical software is becoming a rising problem for healthcare facilities across the US, yet the push for digital patient experiences continues to grow. A CDC study found that 47.7% of adults ages 30-44 use the internet to communicate with a doctor or doctor's office. However, still existing paperwork, manual processes and legacy systems prolong…Learn More
RPA in Healthcare: Smarter Operations for Better Patient Care
The healthcare industry today is not only struggling with growing administrative spending but also with the increasing rates of staff burnout in healthcare facilities due to the high volume of repetitive tasks. As per Statista, 58% of registered nurses report burnout on most days, which results from both excessive emotional stress, the growing workload and…Learn More
Conversational AI for Healthcare: Changing How Patients Experience Care
The U.S. healthcare system has a serious problem with communication and management. Much of the strain comes from staggering administrative burdens. Research shows that physicians may spend nearly half of their clinic day devoted to documentation and non-clinical work. This imbalance damages the quality of care, makes it harder for people to access help, and…Learn More