Cloud Migration for Hospitals Is No Longer Optional: How to Do It Right
Moving to the cloud has become a basic requirement for healthcare providers, not an optional strategy. Most hospitals already run some services in the cloud, yet the journey is far from finished. A number of institutions have shifted specific tasks, such as disaster recovery, to remote servers; a HealthTech poll reports that 63% of IT leaders point to improved reliability and faster recovery as the top benefit. Still, the sector sits low on the cloud‑maturity ladder, meaning that core production systems, including patient records, billing platforms, and analytics tools, need to follow sooner rather than later if hospitals want real flexibility and the ability to scale.
Research tells us that 88% of healthcare providers have sped up their cloud adoption, yet 62% of those initiatives stumble or run into serious problems. The mismatch between what organizations plan and what they actually achieve shows just how tough it is to move sensitive, mission‑critical workflows to the cloud. Hospital executives know why they must act: data silos have to be broken, cyber‑security risks are climbing, and systems need to talk to each other more smoothly.
Getting the cloud right takes more than technical skill. Hospital leaders also need a plan that ties technology choices to both clinical outcomes and the bottom line. The following guide lays out a step‑by‑step roadmap, pointing out common pitfalls and offering practical steps so your organization can complete the migration and start seeing real benefits.
Why is cloud migration now essential for hospitals?
Several urgent pressures are forcing healthcare to look beyond on-premise data centers. What used to be the default setup now brings steep financial costs, security gaps, and operational headaches that contemporary cloud services can ease.
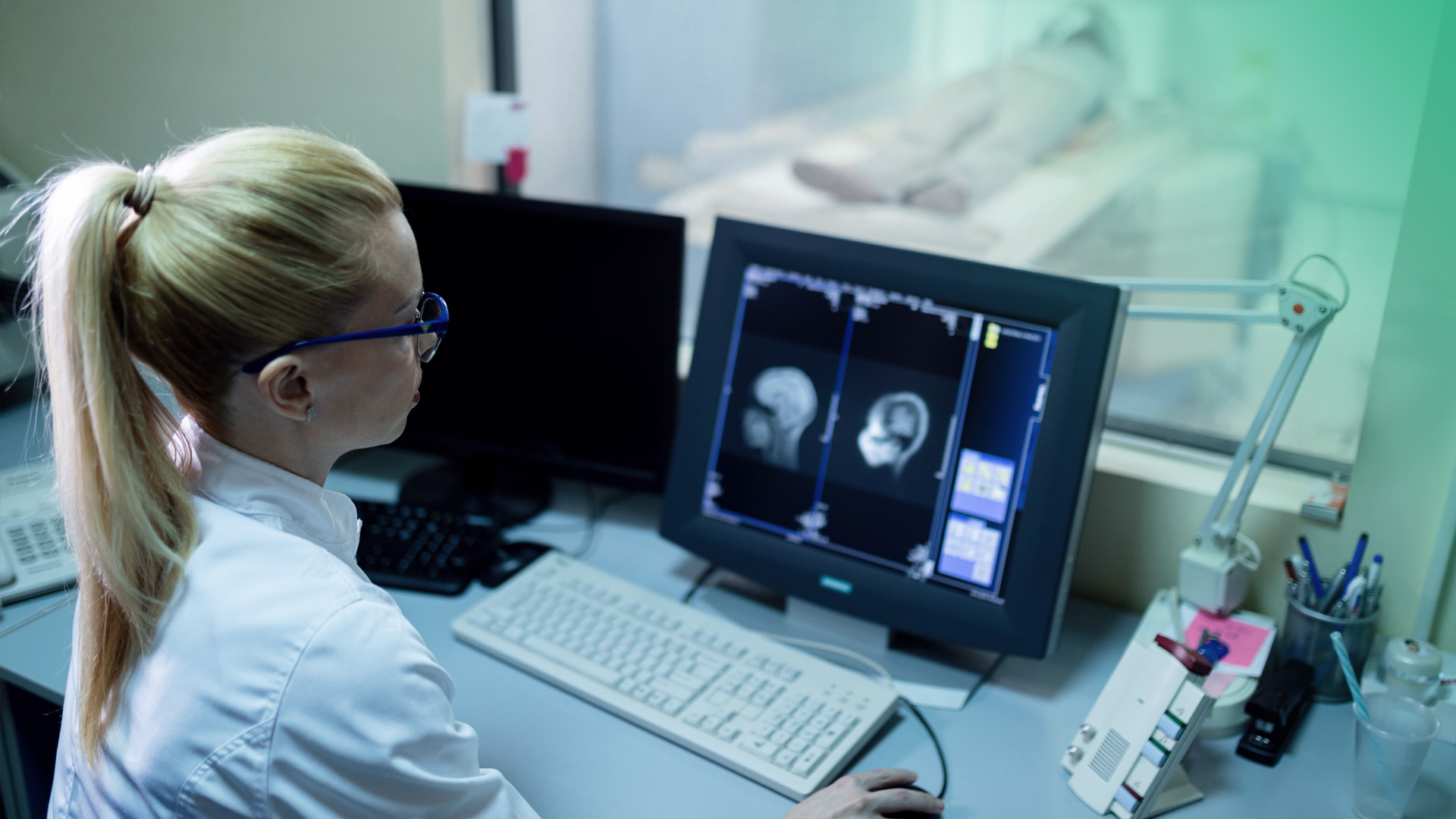
Rising Cybersecurity Threats
Hackers often set their sights on health providers, and ransomware can cripple both operations and patient safety. Individual hospitals struggle to match the security depth that large cloud vendors can offer. According to a Tateeda report, providers such as AWS, Azure and Google Cloud deliver continuous threat monitoring and automatic patching, features designed to safeguard patient information and meet HIPAA requirements.
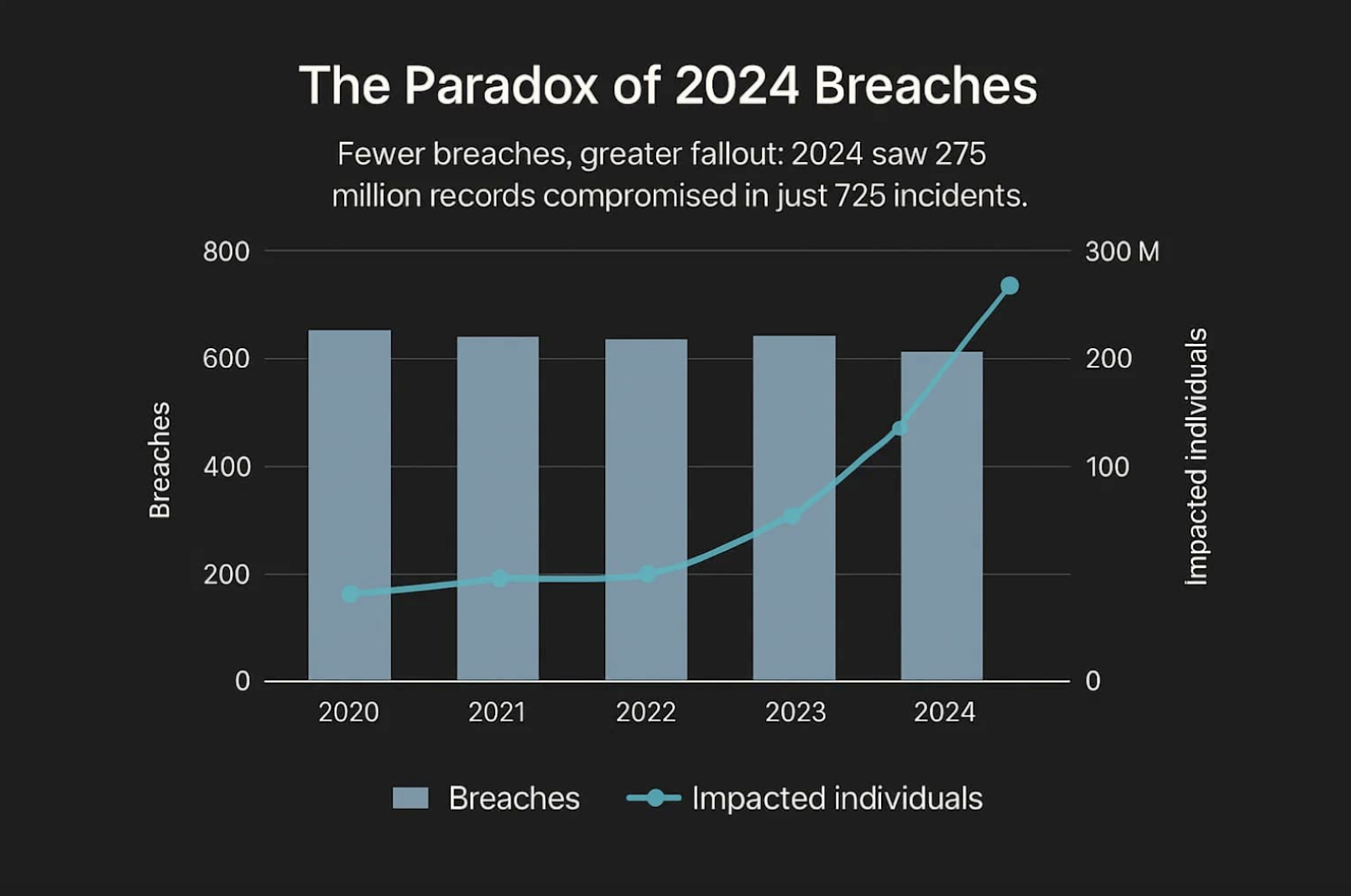
Source: DeepStrike
Increasing Demands for Operational Efficiency
Healthcare operations benefit from rapid scaling. In the cloud, computing expands or contracts as patient volumes shift, covering everything from busy emergency periods to bursts in telehealth appointments. The result is steady performance for both clinical and back-office workloads, with fewer failures than on legacy hardware. The same environment supports secure off-site access and real-time teamwork, making it easier to share data and coordinate treatment.
Significant Cost Pressures and Resource Optimization
Keeping legacy hardware, particularly old mainframes, on site is expensive. Deloitte’s case study shows an academic hospital spending almost $1 million each year on mainframe upkeep, while also struggling to find staff with the needed expertise. After moving those workloads to the cloud, the institution turned hefty financial setbacks into manageable operating expenses and cut total costs by about 95%.
 Source: Deloitte
Source: Deloitte
What are the key benefits of migrating to the cloud?
When a cloud migration goes smoothly, the payoff goes far beyond reduced bills. It improves patient care, strengthens data protection, and opens doors for innovation.
Enhanced Data Security and HIPAA Compliance
Early worries about cloud security have largely disappeared. Major providers, like AWS, Microsoft Azure, Google Cloud, invest heavily in advanced safeguards and offer HIPAA‑eligible services. They sign Business Associate Agreements (BAAs) that spell out their compliance responsibilities. The result is stronger backup, faster disaster recovery, and fine‑grained access controls that protect patient health information.
Unmatched Scalability and Flexibility
The cloud can expand to meet any demand, letting hospitals add capacity whenever needed. This adaptability matters as the volume of EHRs, imaging files, and IoT data keeps rising. It also means hospitals avoid huge upfront hardware purchases and only pay for the compute and storage they actually consume.
Improved Interoperability and Data Access
For years, isolated systems have made it hard for clinicians to see a patient’s full history. A cloud‑based architecture centralizes data and makes it easy to share via standards such as FHIR and modern APIs. The result is a more complete view of each patient, which leads to better decisions and outcomes.
What common challenges do hospitals face in cloud migration?
Even with the upside, migrating to the cloud presents many hurdles. Recognizing what can go wrong is the first move toward fixing it.
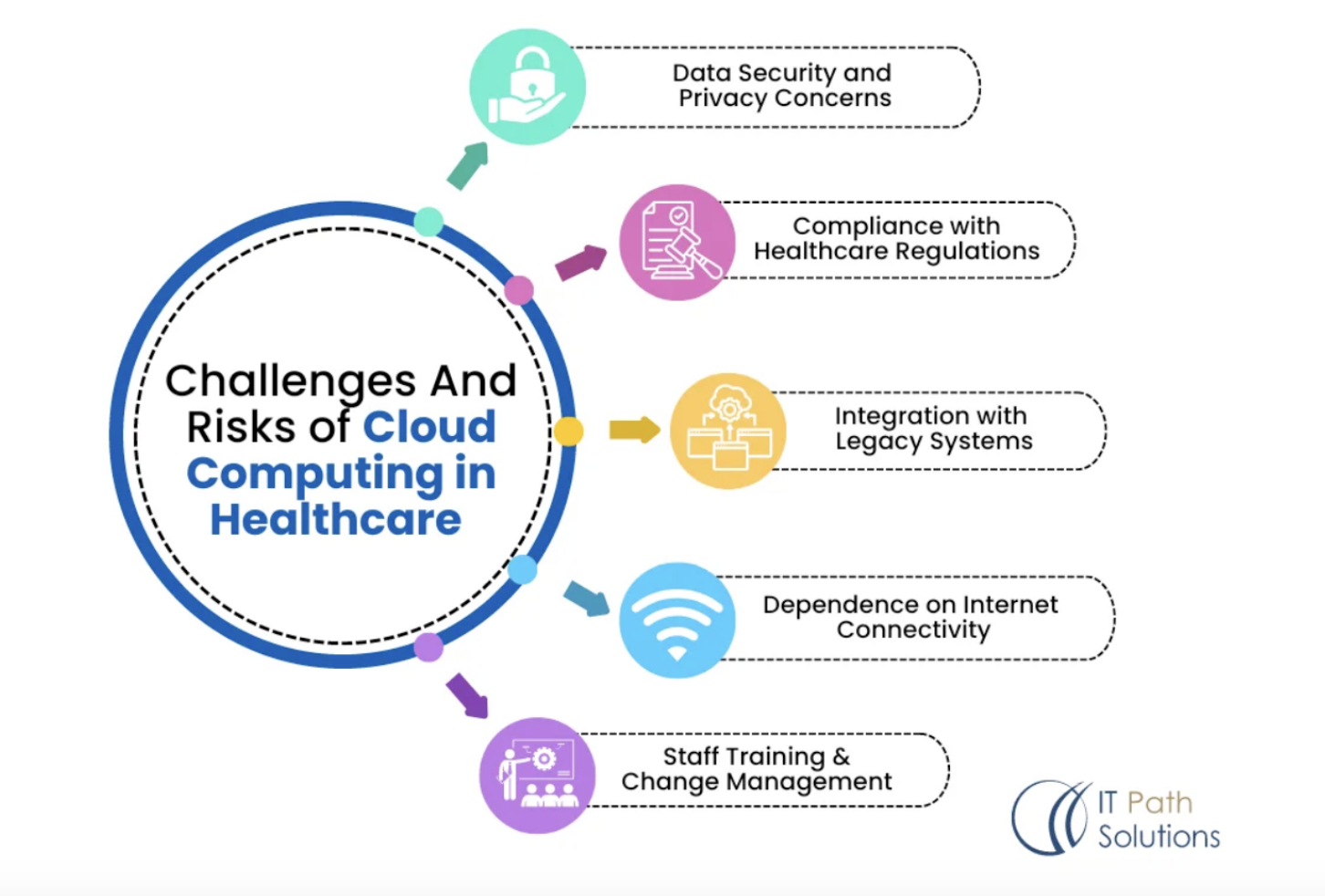 Source: IT Path Solutions
Source: IT Path Solutions
Integrating and Modernizing Legacy Systems
Hospitals often depend on legacy platforms and large monolithic apps that weren’t built for cloud deployment. RT Insights notes that such systems may need extensive code changes, or even a full rewrite, to run smoothly in the cloud. The challenge deepens when documentation is missing, leaving migration teams to piece together architecture and dependencies on their own.
Ensuring Data Integrity and Security During the Transition
Moving data can open new security gaps. Shifting large amounts of patient information demands careful planning to avoid exposure, corruption, or loss. Hospitals should enforce strong safeguards like end-to-end encryption and multi-factor authentication to keep data safe while it travels and when it sits in storage.
Staff Training and Change Management
Even the best technology fails if staff don’t adopt it. A cloud shift brings new tools and processes, which can meet pushback from employees used to older systems. Research published in IJMCER shows that thorough training and transparent communication help ease that friction. Moreover, IT personnel often need to pick up new capabilities in DevOps and cloud security to support the move.
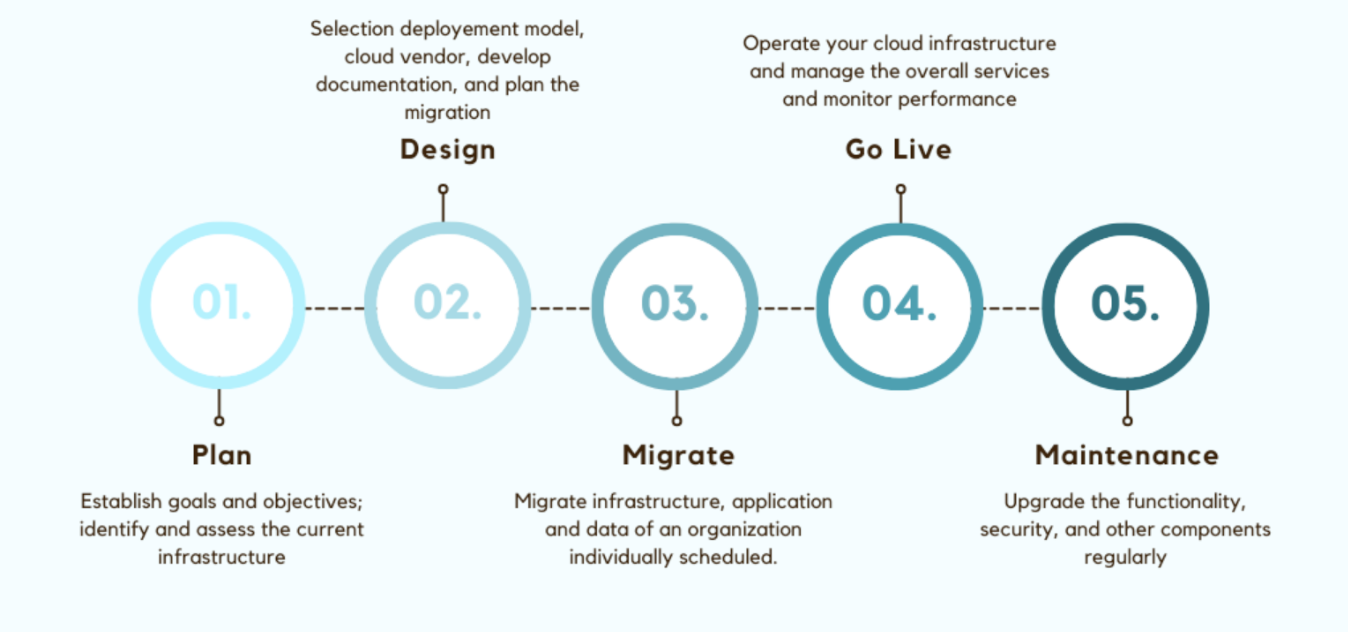
How can you execute a successful migration? A 5-phase roadmap
Breaking the effort into clear phases helps manage complexity, limit risk, and keep the project in line with broader goals.
 Source: DZone
Source: DZone
Phase 1: Comprehensive Assessment and Strategy Development
Everything starts with a deep dive into what you have today and a picture of where you want to be. Begin by auditing the current IT landscape, listing every application, and judging how ready each one is for the cloud. RT Insights stresses that senior leadership, CIO, CFO, and others, must back the effort to tie it to business aims. With that insight, choose the right migration path for each workload, be it lift-and-shift, replatforming, refactoring, or a full replacement.
Phase 2: Detailed Planning and Preparation
Once the overall approach is set, flesh out a step-by-step plan covering schedules, resource assignments, and fallback options. At this point, pick a cloud vendor that satisfies your security and compliance requirements, and that’s willing to sign a BAA. Build a strong governance framework, maybe a dedicated PMO, to give every stakeholder from clinicians to finance, a voice in key decisions.
Phase 3: Migration Execution and Testing
Kick off the move by tackling low-risk apps first, gaining experience and fine-tuning the process before handling mission-critical systems. As each piece goes live, run thorough tests to confirm performance, security, and correct functionality. These checks verify that applications behave as intended and that data remains intact.
Phase 4: Go-Live and Staff Training
When testing is complete, move users onto the cloud platforms. Success hinges on staff readiness. Offer in-depth training that addresses both the new tools and updated security and compliance procedures. Confident users make the change smoother and help sustain adoption over time.
Phase 5: Post-Migration Optimization
Even after the last system is up, the job continues. Keep an eye on performance, security, and spending in the cloud. Adopt FinOps-style cost controls to match resources to demand and avoid runaway bills. Ongoing tuning guarantees you capture the full financial and operational upside.
A Real-World Example: Migrating a National Cancer Care Network to the Cloud
To see how a large‑scale migration works, look at what Kanda Software did for a major national network of cancer care and research centers. The network launched an extensive digital transformation program aimed at getting more out of its technology and improving patient outcomes, and moving everything to a public cloud was a key part of that plan.
Kanda was hired to design and run the cloud migration effort on a leading public cloud platform. The work covered a wide range of tasks: shifting complex online transaction‑processing systems and building roughly 750 ETL (Extract, Transform, Load) pipelines to move huge volumes of clinical and operational data securely.
To give the client a clear view of the new environment, Kanda also created custom reporting dashboards in Tableau and QlikView, delivering the insights needed for effective data management.
The project shows that a close collaboration between the client and a specialist can handle the technical and logistical hurdles of moving highly sensitive healthcare data at scale.
How can Kanda help?
Given the intricacy of hospital cloud moves and the high failure rate, a seasoned technology partner becomes indispensable. Kanda Software offers almost thirty years of experience guiding healthcare organizations through each phase of their cloud transition.
- Build a full migration plan: We evaluate your existing infrastructure, map a step-by-step roadmap from readiness check to final transition, and align the effort with both clinical and financial objectives.
- Carry out data and app migrations: Our engineers handle the technical work, like defining data structures, converting code, and moving legacy systems, while preserving data integrity and keeping patient care disruption to a minimum.
- Protect data and meet HIPAA: We apply strict security measures, like vulnerability management and secure architecture design, to safeguard PHI and maintain HIPAA compliance throughout the migration.
- Maximize cost and performance: We deliver precise cost forecasts, set up controls, and use DevOps-as-a-Service plus continuous monitoring to fine-tune your cloud for optimal performance and spend efficiency after migration.
Talk to our experts to understand how technical depth and strategic insight can reshape your healthcare IT landscape. Discover more about our digital health product and software development capabilities.
Conclusion
Shifting from isolated, on-premise systems to an integrated cloud infrastructure is now a must for hospitals. This evolution boosts security, streamlines operations, and paves the way for truly patient-focused care. Moreover, it creates the foundation needed to adopt advanced tools such as AI and real-time analytics that will shape tomorrow’s medicine.
Yet technology alone won’t carry the journey. Winning outcomes require a solid strategy, careful planning, and thoughtful handling of the human side of change. By recognizing the typical obstacles and following a clear roadmap, often with help from an experienced partner, hospitals can unlock the full value of their data and provide safer, more effective, and better-connected care for all.
Related Articles

7 Ways RAG in AI Models Supports Modern Healthcare
If you’ve read our blog, then the challenges in healthcare IT are familiar ones. Data sits trapped in silos, clinicians lack quick information retrieval when it matters most, and AI tools might produce made-up answers without any warning. Large language models promised to change this, but hallucination remains a serious liability. Mayo Clinic demonstrated the…Learn More
Healthcare Web Development: The Fastest Route to Scalable Patient Care
Outdated medical software is becoming a rising problem for healthcare facilities across the US, yet the push for digital patient experiences continues to grow. A CDC study found that 47.7% of adults ages 30-44 use the internet to communicate with a doctor or doctor's office. However, still existing paperwork, manual processes and legacy systems prolong…Learn More
RPA in Healthcare: Smarter Operations for Better Patient Care
The healthcare industry today is not only struggling with growing administrative spending but also with the increasing rates of staff burnout in healthcare facilities due to the high volume of repetitive tasks. As per Statista, 58% of registered nurses report burnout on most days, which results from both excessive emotional stress, the growing workload and…Learn More
Conversational AI for Healthcare: Changing How Patients Experience Care
The U.S. healthcare system has a serious problem with communication and management. Much of the strain comes from staggering administrative burdens. Research shows that physicians may spend nearly half of their clinic day devoted to documentation and non-clinical work. This imbalance damages the quality of care, makes it harder for people to access help, and…Learn More