Conversational AI for Healthcare: Changing How Patients Experience Care
The U.S. healthcare system has a serious problem with communication and management. Much of the strain comes from staggering administrative burdens. Research shows that physicians may spend nearly half of their clinic day devoted to documentation and non-clinical work. This imbalance damages the quality of care, makes it harder for people to access help, and puts stress on an already stretched system. Healthcare organizations are now looking at conversational artificial intelligence to help manage this pressure. These AI-powered tools can collect information, answer patient questions, and support clinical decisions through natural, context-aware conversations. The goal here isn't to replace doctors, these tools are meant to support healthcare professionals by taking over repetitive tasks, which can make the entire patient experience more efficient and accessible.
What is conversational AI for healthcare?
First, we need to clarify what makes conversational AI different from the basic chatbots most people have dealt with.- Basic chatbots rely on fixed, rule‑based scripts. They push users through static menus (“Press 1 for appointments”). As soon as a conversation veers into medical jargon, slang, or anything beyond their programmed paths, they tend to stall.
- Conversational AI operates on a different level. It uses artificial intelligence techniques to mimic human dialogue and automate interactions. The technology rests on two main building blocks:
- Natural Language Processing (NLP) – Think of this as the system’s “brain.” NLP lets the software parse, comprehend, and generate everyday language. Within it, Natural Language Understanding (NLU) works out the speaker’s intent and context, pulling out details like symptom, description, and duration from a phrase such as “I’ve had a sharp headache for two days.”
- Machine Learning (ML) – This acts as the “engine” that improves the system over time. By exposing the model to large, high‑quality medical datasets, it learns to recognize varied phrasing, follow complex clinical discussions, and deliver more precise answers.
How is conversational AI transforming patient care?
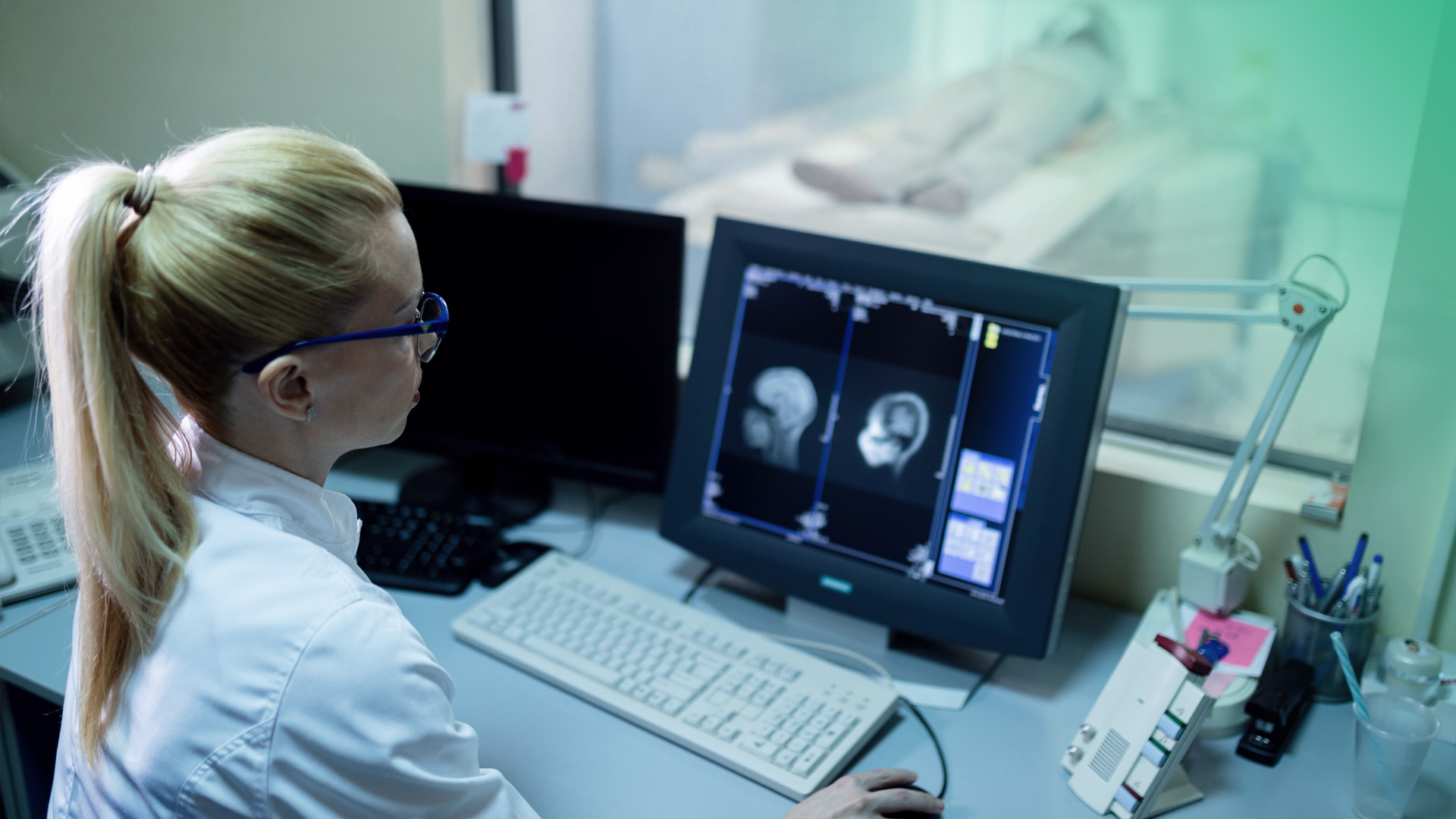
Conversational AI isn't just handling back office tasks. It's directly improving clinical outcomes and the services patients actually interact with.Patient Triage and Symptom Assessment
AI-powered systems can work as an intelligent, scalable entry point for a health system. Instead of waiting on hold or trying to figure out where to go, patients can talk to an AI that has an actual conversation with them. The AI asks follow-up questions to figure out how severe the symptoms are and how urgent the situation is. Based on what it learns, the AI points the patient toward the right kind of care, whether that's a telehealth visit, a primary care appointment, an urgent care visit or an ER visit for something more serious. This takes some pressure off overwhelmed emergency departments, which often struggle to separate real emergencies from cases that could be treated somewhere else.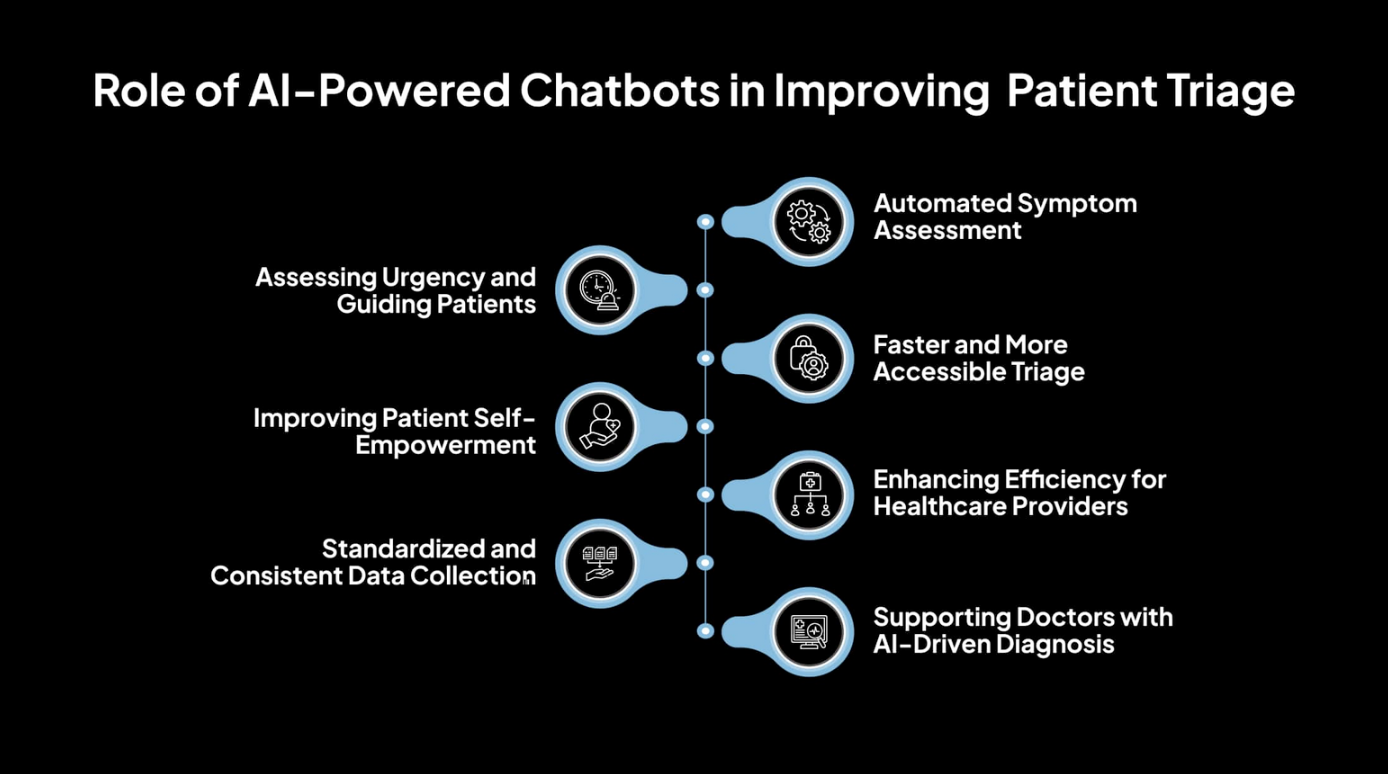 Source: Avahi
Source: Avahi
Medication Adherence and Remote Monitoring
Medication non-adherence is a big, expensive problem. Studies show that up to 50% of patients with chronic illnesses don't take their medications the way they're supposed to. Conversational AI provides a more interactive way to handle this. Instead of just a basic alarm, an AI assistant can send a reminder that feels more like a conversation: "Hi, it's time for your medication. Have you taken it?" If the patient has questions or mentions a side effect, the AI can offer helpful information or alert a real clinician. This works especially well for managing chronic diseases and checking in after hospital discharge. Active monitoring like this can catch problems early and cut down on readmissions.Mental Health Support and Wellness Coaching
The demand for mental health services significantly exceeds the available number of providers. Conversational AI can help close that gap by offering accessible, round-the-clock support that doesn't judge. The anonymity of talking to an AI can lower the stigma that keeps a lot of people from getting help. These tools can walk users through evidence-based techniques, like Cognitive Behavioral Therapy (CBT) exercises for managing anxiety or changing negative thought patterns. More advanced systems can even pick up on crisis signs by analyzing voice patterns and emotional cues, then escalate serious situations to a human.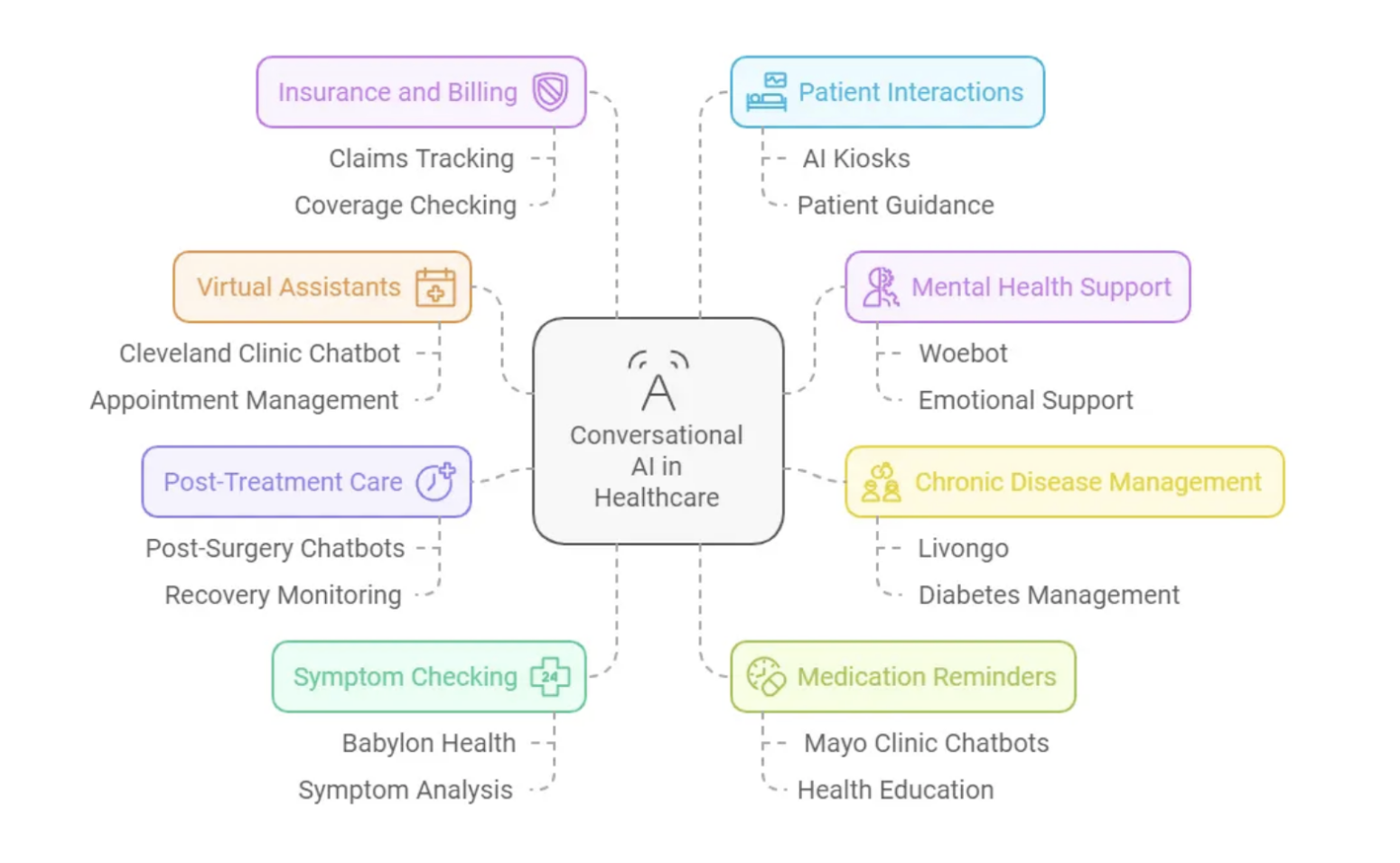 Real-world examples of conversational AI in healthcare.
Source: Desku
Real-world examples of conversational AI in healthcare.
Source: Desku
What administrative tasks can AI automate?
One of the biggest and fastest benefits of conversational AI is how it cuts down on the overwhelming administrative work that burns out clinicians and drives up costs.Appointment Scheduling and Management
Booking, canceling, and rescheduling appointments consumes a lot of time for front desk staff. Conversational AI can automate all of that. Patients can use an AI bot on the web or phone to find and book times whenever they want, day or night. The system can also send out reminders, which cuts down on no-shows and frees up staff to handle more complicated patient needs.Insurance Verification and Pre-Authorization
Prior authorization has been called healthcare's administrative nightmare, and for good reason. It often delays critical care for days or even weeks. AI-powered tools can speed this up by running real-time insurance eligibility checks automatically. More sophisticated systems can review clinical documentation, pull out the relevant medical reasoning, and generate prior authorization requests on their own. That cuts down on errors and claim denials.Patient Intake and Documentation
Conversational AI can get rid of the old clipboard routine. Before a visit, an AI tool can securely message patients to collect intake information like symptoms, medical history and insurance details. The most game-changing use here is ambient clinical documentation. An AI-powered device in the exam room listens securely to the conversation between doctor and patient. It automatically transcribes the whole encounter from history, to exam findings and care plan, and transcribes it straight into the fields in the patient’s Electronic Health Record (EHR). This lets the doctor focus completely on the patient instead of staring at a screen, fighting provider burnout.How can healthcare organizations successfully implement it?
Deploying conversational AI isn't as simple as flipping a switch. It takes a real strategy for integration, security, and managing data.EHR Integration and Data Security
One of the common challenges with new healthcare tech is getting it to work with old legacy systems. For an AI tool to actually be useful, it must integrate seamlessly with the organization's EHR. That takes solid technical architecture, usually built on modern APIs and healthcare standards like FHIR (Fast Healthcare Interoperability Resources). Data security isn't optional. Any system touching patient information has to be fully HIPAA-compliant. That means strong end-to-end encryption, tight access controls, and regular security audits to keep sensitive patient data safe.Training AI Models on Medical Terminology
In healthcare, precision is everything. A standard AI simply isn't built for these high stakes. Ask a generic model about "atrial fibrillation," and you might get a response that’s not just wrong, but clinically nonsensical. Healthcare AI has to be in a different league entirely. It needs medical grade intelligence, built and trained on vast, specialized vocabularies to interpret complex medical language with unerring accuracy. The training data is also a critical ethical issue. A 2024 study in PLOS Digital Health points out growing concerns that AI tools could maintain or even worsen health inequalities if they're not designed carefully. If the training data isn't diverse, the AI might work worse for minority populations. That means equity has to be a priority and using high-quality, diverse datasets is crucial.How do you measure success and ROI?
For healthcare executives and IT directors, measuring success means looking at clear, concrete metrics.- Operational Efficiency: This covers things like less administrative work for staff, fewer phone calls to handle, and measurable time saved on scheduling, intake, and billing.
- Financial Impact: ROI shows up in lower operational costs, fewer patient no-shows, fewer denied claims, and fewer expensive 30-day readmissions.
- Patient Experience: Success here means better patient engagement and higher satisfaction scores.
- Clinical Outcomes: Key numbers to watch include better medication adherence and improved outcomes for patients managing chronic diseases.
What are the challenges and limitations?
The technology shows a lot of promise, but it's not a cure-all. Building trust means being honest about what it can't do.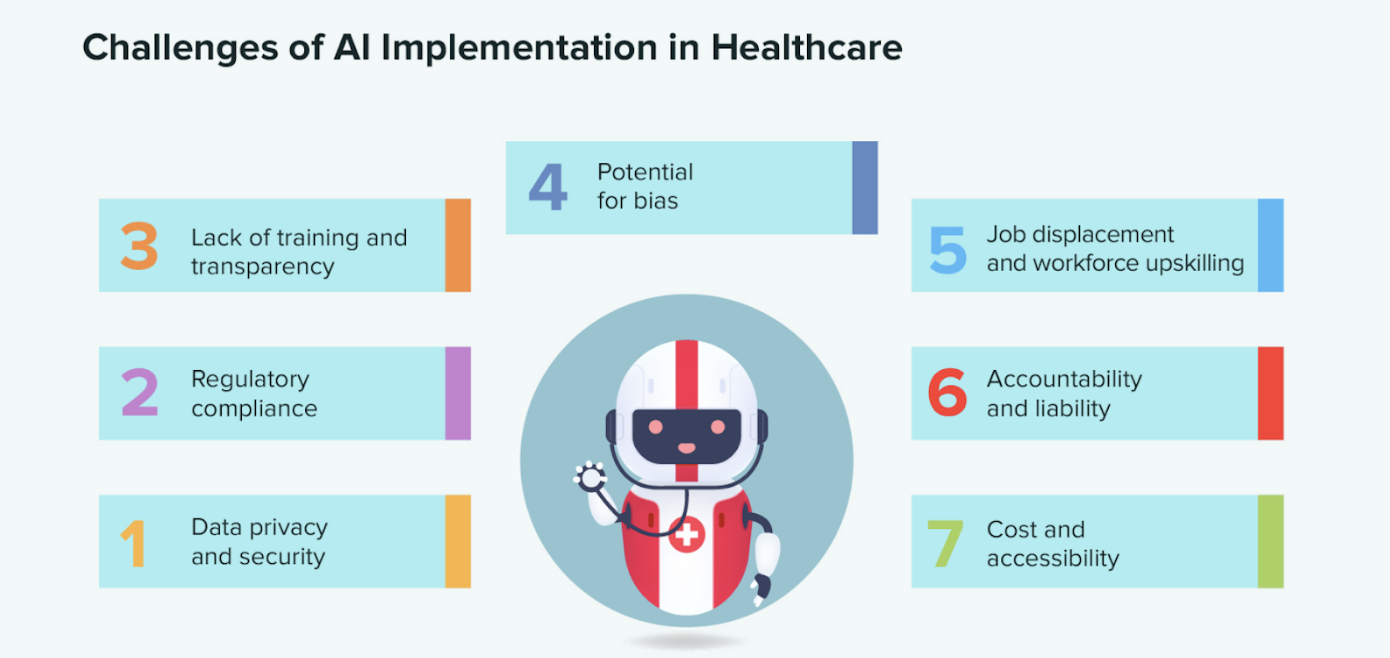 Source: Svitla
Source: Svitla
- Technical and Safety Hurdles: Latency, or those awkward pauses in conversation, can quickly erode a user's trust. On top of that, advanced AI can be unpredictable. It can "hallucinate" and generate responses that are clinically wrong or biased. This is why it’s extremely important to build rigorous auditing and quality-control processes with an experienced development partner who understands both the clinical and AI side of things.
- Adoption Barriers: Some patients just prefer talking to a real person. Staff adoption can be tough too. Oftentimes new adopters worry that new tools will just pile on more work. Getting past this takes thorough training and showing that the tool is there to help, not replace anyone.
- Ethical Concerns: The risk of algorithmic bias is real and serious. A roadmap for equitable AI in PLOS Digital Health stresses that developers need to actively partner with diverse and underrepresented communities to build these tools together. Otherwise, they risk baking existing health disparities right into the technology. Partnering with a trusted and experienced service provider will ensure all your bases are covered.
How Kanda Can Help
Getting conversational AI working in a clinical setting is complicated. It takes real expertise in AI, data security, and the specific workflows of healthcare. Kanda can help with:- Building Custom, HIPAA-Compliant Platforms: We design secure, scalable, compliant conversational AI solutions built around your specific clinical and administrative requirements.
- Managing Complex EHR Integration: Our team builds solid data pipelines and uses FHIR standards to make sure your AI tools work smoothly with your existing EHR and legacy systems.
- Developing and Training Medical-Grade AI: We don't use generic models. We apply our AI and machine learning expertise to train models on specialized medical terminology for complete, auditable accuracy.
- Delivering Full-Stack Healthcare Solutions: From custom software development to the final patient-facing app, we handle the whole healthcare software development process.
Conclusion
Conversational AI is quickly shifting from a new idea to something healthcare really needs. Basic chatbots haven't delivered much value, and the real change is coming from advanced, generative AI platforms that are secure, smart, and built right into clinical workflows. Think of this technology not as a replacement for clinicians, but as a powerful partner. It handles the relentless administrative work, clearing the way for clinicians to dedicate their full attention to patient care. With a smart, secure, and equitable implementation plan, healthcare organizations can transform the patient journey into one that is seamless, supportive, and profoundly human.Related Articles

7 Ways RAG in AI Models Supports Modern Healthcare
If you’ve read our blog, then the challenges in healthcare IT are familiar ones. Data sits trapped in silos, clinicians lack quick information retrieval when it matters most, and AI tools might produce made-up answers without any warning. Large language models promised to change this, but hallucination remains a serious liability. Mayo Clinic demonstrated the…Learn More
Healthcare Web Development: The Fastest Route to Scalable Patient Care
Outdated medical software is becoming a rising problem for healthcare facilities across the US, yet the push for digital patient experiences continues to grow. A CDC study found that 47.7% of adults ages 30-44 use the internet to communicate with a doctor or doctor's office. However, still existing paperwork, manual processes and legacy systems prolong…Learn More
RPA in Healthcare: Smarter Operations for Better Patient Care
The healthcare industry today is not only struggling with growing administrative spending but also with the increasing rates of staff burnout in healthcare facilities due to the high volume of repetitive tasks. As per Statista, 58% of registered nurses report burnout on most days, which results from both excessive emotional stress, the growing workload and…Learn More
Health Insurance Software Development: AI for Prior Authorization
Prior authorization (PA) was supposed to serve as a safety net, checking that patients get the right treatment while keeping costs in check. In reality, it now sits among the biggest administrative hurdles in healthcare. The contrast is stark when you consider how fast the market is growing. The U.S. healthcare software-as-a-service sector was worth…Learn More